“In earlier times, they had no statistics, and so they had to fall back on lies.”
-Original author unknown
—
Hey everyone,
Last time we spoke, I promised my next article would discuss the type of diet that’s been shown in clinical trials to reduce cardiovascular mortality. However, something else has crossed my desk that I need to comment on pronto.
As a result, this article is going to be about a type of eating pattern that, despite all the lavish claims made for it, has never been shown to reduce CVD mortality in clinical trials. In fact this style of eating, despite the reigning propaganda, has never been shown to reduce death from any cause.
I’m talking, dear readers, about vegetarianism.
An EPIC Wank
Late last year a big ballyhoo was made about an analysis of the large EPIC-Oxford epidemiological study in England that compared cardiovascular outcomes in those who called themselves vegetarians with those who did not. As I explained in this article, an earlier analysis of the EPIC-Oxford cohort found no reduction in cardiovascular mortality among vegetarians. It did, however, find that overall mortality was slightly albeit non-statistically significantly higher among this group. For some strange reason, this study attracted very little attention from the media.
Not content with these uninspiring results, the EPIC researchers – two of whom belong to organizations whose express purpose is to promote vegetarianism – decided to conduct another analysis, this time combining both fatal and non-fatal cardiovascular outcomes. Analysing each of these outcomes alone had failed to produce any kind of statistically significant risk reduction, but using the old trick of combining endpoints finally produced a result that could be used to further the vegetarian cause. The researchers promptly drafted another paper completely ignoring the previous unfavourable all-cause mortality results, instead gushing on about the “reduced risk” of combined fatal and non-fatal heart disease. Media outlets all around the world quickly proceeded to insult our intelligence with headlines such as “Vegetarian diets reduce heart disease risk by a third.”
Hmmm, I guess they never received any glowing press releases for the previous EPIC paper showing no reduction in CVD mortality, a higher rate of colorectal cancer, and a slightly higher rate of overall mortality among vegetarians. And I guess no-one ever explained to them that the only reason vegetarians enjoyed any reduction in CVD was their significantly younger mean age, their lower rate of smoking, and higher rates of exercise.
Funny that.
I debunked that study here, and explained why vegetarian diets are more likely to promote rather than prevent cardiovascular disease. Today, I’m going to dismantle another audaciously misleading pro-vegetarian paper.
When Religion Combines with Diet Dogma – Literally
So let’s leave the UK, and travel over to the US where there resides another group of researchers conducting a large-scale epidemiological comparison of vegetarians and omnivores.
The population being studied is comprised of Seventh Day Adventists, a religious denomination that advises its members to follow a vegetarian diet. From all accounts, this admonition is not administered with quite the same vigour as, say, the Jewish and Muslin proscriptions against pork. And so not all Adventists follow a truly vegetarian diet, allowing researchers to follow what would appear to be a relatively homogenous population consuming various levels of animal products.
This page contains “The Seventh-day Adventist Position Statement on Vegetarian Diets”, and states:
“The vegetarian diet recommended by Seventh-day Adventists includes the generous use of whole grain breads, cereals and pastas, a liberal use of fresh vegetables and fruits, a moderate use of legumes, nuts, seeds. It can also include low fat dairy products such as milk, yogurt and cheeses and eggs. It is best to avoid high saturated fat and cholesterol foods such as: beef, lamb, pork, chicken, fish and seafood. Coffee, tea and alcoholic beverages provide few nutrients and may interfere with the absorption of essential nutrients.”
It goes on to claim:
“Vegetarians have reduced risks of certain diseases because of their increased consumption of whole grains, dried beans, nuts, fresh and dried fruits, and vegetables. Vegetarians are exposed to fewer carcinogens and mutagens because they do not eat meat.”
Here’s the truth: There exists no reliable evidence whatsoever that avoidance of meat reduces the incidence of cancer nor any other disease. As for the 7DA proscription against tea and coffee, both are antioxidant-rich beverages that show little evidence of harm when consumed in sensible amounts. Heck, even epidemiologists struggle to find harmful associations between tea, coffee and health and mortality outcomes; quite the opposite, in fact[1].
It’s also most ironic that whoever drafted this position statement criticizes tea and coffee for their alleged nutrient-inhibiting effects when whole-grains contain a plethora of what researchers refer to as anti-nutrients, which have been well documented to inhibit the absorption or production of such critical nutrients as zinc, magnesium, calcium, selenium, and vitamins B6 and D. Unlike tea, which clinical trials indicate is a most health-enhancing beverage, controlled trials have repeatedly shown increased whole-grain consumption to produce negative health outcomes.
Hmmm. A religious organization making claims with no foundation in sound science. Gee, who would’ve thought?
As to why the 7DA religion settled on this eating style in the first instance:
“For more than 130 years Seventh-day Adventists (SDAs) have practiced a vegetarian dietary lifestyle because of their belief in the holistic nature of humankind. Whatever is done in eating or drinking should honor and glorify God and preserve the health of the body, mind and spirit.”
I’ll leave aside the fact that after thousands of years, none of the worshippers of the various “Gods” has been able to provide anything resembling proof for the existence of said Gods. And therefore that eating or drinking with the goal of “honouring” and “glorifying” any of these Gods might not be the most intelligent way to determine one’s eating patterns.
Some people worship Elvis. You might think that’s strange, but at least they can prove he existed LOL
Nope, I won’t bang on about that because, ultimately, people are free to believe whatever they want. If you want to believe in virgin births, resurrections from the dead, or that a bunch of invisible goblins lives under your kitchen table, then good for you. Ditto if you choose to believe avoiding meat somehow affirms the “holistic nature of humankind”, despite the fact that Paleolithic humans – who didn’t just talk the talk but really did live in harmony with nature (like they had a choice) – ate meat on a very regular basis with remarkable evolutionary success for some 2.4 million years.
As anyone who has studied both Paleontology and the history of vegetarianism will know, the latter was quite literally born out of religion. Archaeological evidence, along with observation of surviving hunter-gatherer societies, invariably indicates animal flesh (especially fat-rich animal flesh) was an important and highly valued component of the human diet. It wasn’t until Homo sapiens moved from a nomadic hunter-gatherer existence to a sedentary agrarian lifestyle that they had the time to sit around, gaze at their navel, and dream up concepts such as “non-violent” food acquisition. The first ‘enlightened’ thinkers that came up with this concept were probably written off as a bunch of soft-cocks by their hardy peers, but vegetarian ideologies eventually gained traction, especially when the ruling classes realized the potential advantages to be conferred by forbidding meat consumption in areas where grain cultivation was a much less ecologically expensive method for sustaining rapidly expanding populations.
Those who want to explore this phenomenon further are highly advised to consult the outstanding Cannibals and Kings by Dr Marvin Harris. My goal here is to simply point out that vegetarianism came into being as an ideology among sedentary, agrarian ‘thinkers’. Thousands of years later and little has changed. Vegetarianism is still an ideology with no foundation in anything resembling sound science.
Which would be all fine and dandy if the promoters of vegetarianism stuck to their theoretical ethical musings and made no pretence about the healthfulness of their diet being supported by sound science.
Which in turn brings up a second important point about vegetarianism. It was born from theories about “peaceful” food acquisition and non-violence towards animals which, no matter how admirable their intent, can hardly be considered end-products of the scientific method. Claims for the alleged health benefits of vegetarianism came later. And the science for that came much, much later again.
I’ll repeat: The ideology came first, the science came after.
My long-time readers will be familiar with how this works (think cholesterol hypothesis of heart disease): A theory is constructed based on someone’s interesting but unfounded ideas. The theory holds appeal but the supportive scientific evidence is lacking so researchers go about amassing it after the fact. Instead of testing the hypothesis with ruthless impartiality, the subsequent research is constructed and interpreted in a manner that will support the pre-existing beliefs.
By now you should be starting to see where I’m heading with all this. It’s hardly a secret the Seventh Day Adventist religion has a bias towards vegetarian eating. It makes claims about this style of eating which are of questionable veracity, but when challenged can cite scientific research that supposedly proves its vegetarian exhortations are backed by more than religious commandment.
But guess what?
The same studies examining Adventists and claiming beneficial findings for vegetarian diets are also conducted by Adventists. Specifically, the team of researchers housed in the “Adventist Health Studies” department in the School of Public Health at Loma Linda University.
Loma Linda is home to one of the largest 7DA congregations in the world, and the university is owned by the 7DA church. This university has treated us to a string of papers over the years, many hailing the risk reductions in death and disease that allegedly accompany a vegetarian diet.
Given the longstanding and well documented concerns arising from research conducted by individuals with a vested interest in the results, I’d say a very strong dose of scepticism is warranted when analysing their papers.
Before we take a look at the most recent paper from this team, let’s take a quick look at some of their Greatest Hits from the 70s, 80s, and 90s.
C’mon Baby Lay Your Stats on Me
In 1975, the Loma Linda researchers presented mortality data from over 35,000 Seventh-Day Adventists whom they monitored during the period 1958-1965. Sure enough, this group showed reduced rates of mortality from a number of cancers, but many of these were readily explained by a lower prevalence of smoking and alcohol consumption. Furthermore, the incidence of prostate cancer, which is typically attributed to the consumption of high fat animal foods, was similar between Adventists and non-Adventists.
In addition, recent converts showed a lower risk of breast and colon cancer than life-time Adventists. If animal foods truly contributed to such malignancies then the opposite should have been evident; risk should have declined with increasing length of time as a practicing Adventist.
It has long been recognized that, within populations, individuals from higher socioeconomic backgrounds with higher educational qualifications tend to experience lower rates of various degenerative illnesses than less-educated folks of lower socioeconomic standing. Because Seventh-Day Adventists were generally higher educated than average, the researchers also compared the cancer and all-cause death rates of Adventist and non-Adventist physicians, two groups with very similar educational and career status. They examined the incidence of mortality among over 6,000 medical practitioners who graduated between 1901 and 1971 from Loma Linda University (where over 75% of the graduates were Adventists) and the University of Southern California (where less than 5% of graduates were Adventists).
As expected, the death rate among physicians was lower than the general population, but the “startling” finding was that there was little difference in the rate of cancer or all-cause mortality among the two groups. In fact, the Loma Linda graduates showed a trend towards higher rates of gastro-intestinal and colon cancers, again contradicting prevailing beliefs about the role of animal foods in cancer promotion.
Finally, the researchers examined the relationship between diet and the incidence of colon and breast cancer within the Adventist population itself. Adventists with colon cancer were found to consume more meat, fish and cheese, seemingly supportive of the vegetarian hypothesis. However, colon cancer patients also ate significantly more highly-processed and nutrient-depleted fodder such as ice cream, fried potatoes, fried foods, cakes, and pies. The patients also ingested less green leafy vegetables than cancer-free Adventists. In other words, it was the overall dietary pattern of these patients – one featuring a higher proportion of refined junk – that was associated with colon cancer, not simply the presence of animal foods. Indeed, when the researchers examined the role of each food in isolation, the association between meat, fish and colon cancer disappeared[2].
Consider also a more recent study of over 34,000 Californian Seventh-Day Adventists, published in 1999, which found that vegetarians had lower risks of hypertension, diabetes, arthritis, colon cancer, prostate cancer, fatal CHD in males, and death from all causes. Again, vegetarians displayed a number of healthful dietary habits unrelated to meat intake that were not shared by their omnivorous brethren. Vegetarians consumed more tomatoes, nuts, and fruit, but less donuts than non-vegetarians. Non-vegetarian Seventh-Day Adventists also consumed alcoholic beverages twenty times more frequently than their vegetarian counterparts[3].
As with the earlier study of Adventists published in 1975, these observations clearly showed that those who shunned meat also adopted other dietary measures that protected their health.
Before we discuss more Loma Linda findings, let’s catch another flight, this time over to Norway to check out some research on 7DAs conducted by non-7DA researchers at the University of Tromso.
They studied the mortality pattern of SDAs in the Netherlands during the period 1968-1977. Standardized Mortality Ratios for total mortality, cancer and cardiovascular diseases were significantly lower than for the total Dutch population. Mean age at death as well as life-expectation at baptism were significantly higher in SDAs, both in males and females, compared with Dutch males and females.
To try and find out why, the researchers administered a health survey among a sample of the SDAs population and a group of “friend controls”.
These researchers, who presumably had little incentive to prop up the vegetarian sham, concluded that abstinence from cigarette smoking was likely the main factor explaining the low mortality from ischaemic heart diseases among SDAs, while “presumably an appropriate (prudent) diet confers additional benefit for example on colon cancer mortality”[4].
Notice the emphasis on smoking, and also note how they refer to a “prudent” diet, rather than a vegetarian diet.
In a later study by the same department, little difference in cancer incidence was found between 7DAs and the general population. Total mortality was significantly lower only in 7DA men, especially cardiovascular mortality. They found entering the church at an early age had a large effect on later mortality. They concluded “An early establishment of a healthy lifestyle seems to be of decisive importance in the risk of later disease.”[5]
Notice the emphasis on a “healthy lifestyle”, as opposed to diet.
Ok, now back to California. In their earlier reports, the Loma Linda researchers occasionally dropped their guard and also presented findings supporting the thesis that an overall healthier lifestyle rather than a vegetarian diet was what really explained any lower incidence of disease and mortality.
A 1984 paper, for example, reported lower breast cancer mortality among 7DA women. But, in the researchers own words: “The differences, however, were no longer significant when stage at diagnosis was taken into account. It seems likely that the lower breast cancer death rates reported among Seventh-day Adventist women as compared with the general population result in part from better survival patterns due to earlier diagnosis and treatment.”[6]
Gary E. Fraser, a prominent member of the Loma Linda pro-vegetarian research team, wrote in 1988:
“The lower risk for IHD [ischaemic/coronary heart disease] in Adventist men, at least, is probably related to their dietary habits, nonsmoking status, possibly their better exercise habits, and greater social support.”[7]
That’s a lot closer to the truth than some of his more recent conclusions, but let me re-word the above sentence so that it’s even more in accord with valid science:
“The lower risk for IHD in Adventist men has nothing to do with avoidance of meat, but everything to do with their far lower rates of smoking, greater participation in exercise, maintenance of a lower BMI, and quite possibly the stress-buffering effects of greater social support.”
The following year, Fraser and his colleagues published a paper examining prostate cancer risk among some 14,000 Seventh-day Adventist men who completed a detailed lifestyle questionnaire in 1976 and who were monitored for cancer incidence until the end of 1982. Now, before I relay their findings, remember that meat and animal fats are incessantly blamed for causing prostate cancer.
So what did they find?
–“Increasing educational attainment was associated with significantly decreased risk of prostate cancer in this study.” Nothing to do with diet, obviously.
–“age at first marriage was also inversely associated with risk, although this was not significant” (and also totally unrelated to diet).
–“A history of prostate “trouble” was associated with a 60% increase in risk which was highly significant.”
–“Although there were suggestive relationships between increasing animal product consumption and increased risk, these results did not persist after accounting for the influence of fruit and vegetable consumption. Nor was exposure to the vegetarian lifestyle during the childhood years associated with alterations in subsequent risk. However, increasing consumption of beans, lentils and peas, tomatoes, raisin, dates, and other dried fruit were all associated with significantly decreased prostate cancer risk.”
That same year they also examined the link between diet and breast cancer. They found:
“Age at first live birth, maternal history of breast cancer, age at menopause, educational attainment, and obesity were all significantly related to risk. However, increasing consumption of high fat animal products was not associated with increased risk of breast cancer in a consistent fashion. Nor were childhood and early teenage dietary habits (vegetarian versus nonvegetarian) related to subsequent, adult risk of developing breast cancer. Also, a derived index of percent of calories from animal fat in the adult years was not significantly related to risk. These results persisted after simultaneously controlling for other, potentially confounding variables, utilizing Cox proportional hazard regression models.”[8]
In other words, in these studies consumption of animal foods and SFA (Saturated Fatty Acids) had SFA to do with the likelihood of getting prostate or breast cancer. It was other health and lifestyle characteristics that explained the difference.
Another paper from 1988 is worth mentioning here. It also found a similar lack of risk from animal foods and breast cancer mortality, but a look at the relative risks is good for a chuckle:
“Odds ratios of 1.00, 1.22, and 1.03 were observed for meat consumption categories of none or occasional, 1-3 days/week, and 4+ days/week, respectively.”[9]
If we’re to take this epidemiological pap seriously, then avoidance of meat, milk, cheese, and eggs confers zero increase in fatal breast cancer risk, rises by 22% in relative terms with consumption 1-3 days/week, but then pretty much returns to zero with consumption 4 or more days/week.
Yeah, that makes sense…
A little later, in 1994, the researchers found no difference in cancer incidence between 7DA and non-7DA, except for endometrial cancer which was significantly higher among 7DA women. Overall cancer mortality was lower in 7DA men, with the exception of prostate cancer, which was significantly higher[10]. If we’re to attribute the lower cancer incidence of 7DA men to diet, then it’s only fair we also ascribe the higher incidence of prostate cancer to their eating habits.
Personally I think all this epidemiology is a load of confounder-prone bollocks, and I’m not prepared to ascribe jack to jack until a little later when we look at the RCT data.
For now, let’s jump forward to the present, and check out the paper the Loma Linda researchers published earlier this year. While it didn’t get quite the same level of coverage as the EPIC paper from last year, this paper was still awarded misleading headlines from unthinking journalists, including these gems:
“Vegetarian diet may reduce risk of early death” – CBS News
“Lower risk of death is associated with vegetarian diets” – Examiner.com
“Are vegetarian diets secret to long life? People who avoid meat have better health due to lower blood pressure” – Daily Mail UK
Holy beefsteak, Batman.
My dear readers, I have a dream…that our children will one day live in a world where the media forbids health and nutrition stories to be written by anyone other than those who have a clue about health and nutrition and also know how to impartially read and pick apart a scientific paper.
Because as it stands, most journalists who write diet and health articles don’t have the first clue about diet and health, nor do they even bother to read the studies they report on. Instead they rely on the hyperbolic press release issued by the research team or the medical journal in question. If they need further information to pad out their article, instead of doing their own research they’ll simply contact the head researcher for a bunch of quotable quotes.
While this journalistic cluelessness makes life a lot easier for purveyors of dietary disinformation, it sucks massively for all those who would like their dietary information to be of the factual, scientifically valid, non-BS variety.
And make no mistake: The claims made for the latest study out of Loma Linda are complete BS.
The Bizzarro World of Statistics: When a Lower Risk of Mortality is a Higher Risk of Mortality.
This most recent 7DA paper, published in the JAMA Internal Medicine on June 3, reported on 73,308 participants from the Adventist Health Study 2 (AHS-2) who, based on their questionnaire responses, were categorized into 5 dietary patterns: nonvegetarian, semi-vegetarian, pescovegetarian, lacto-ovo–vegetarian, and vegan[11].
The researchers claim:
“The adjusted hazard ratio (HR) for all-cause mortality in all vegetarians combined vs nonvegetarians was 0.88…The adjusted HR for all-cause mortality in vegans was 0.85…in lacto-ovo–vegetarians, 0.91…in pesco-vegetarians, 0.81…and in semi-vegetarians, 0.92 compared with nonvegetarians. Significant associations with vegetarian diets were detected for cardiovascular mortality, noncardiovascular noncancer mortality, renal mortality, and endocrine mortality.” (All these findings statistically significant at 95% confidence interval).
You’ll note their repeated use of the word “adjusted”; we’ll explore the significance of this in a moment.
In the meantime, this study has so many flaws it’s hard to know where to start.
I could elaborate on what a joke it is to claim ‘significance’ for a 12% risk reduction from a confounder-prone epidemiological study (in randomized controlled clinical trials, such miniscule RRs are routinely dismissed as too weak to get excited over, and we’re talking studies with far less confounding than the epidemiological slop being served up to us by the Loma Linda team).
I could also elaborate on the sheer stupidity inherent in the term “pescovegetarian”. Let’s get something straight – if you eat fish, you ain’t no vegetarian. If you’re going to stick with this high and mighty moral routine that forbids the killing of living creatures, then plain basic logic dictates you must acknowledge fish are also living creatures that must be killed in order for you to consume them. After all, how can it be in harmony with “the holistic nature of humankind” to avoid killing land-based animals for food, but to go ahead and kill aquatic creatures for the exact same purpose?
I could elaborate on these things and more, but I won’t. Instead I’m going to plunge a cyber-knife right into the guts of this study and expose it outright for the utter fraud it is.
And make no mistake: Any claim this study demonstrates lower mortality among vegans, vegetarians, fish eaters (the so-called “pescovegetarians”) and semi-vegetarians is a patently fraudulent one.
Why?
Because that’s what the researchers’ own data shows. The raw data, that is. The actual, unmolested figures the researchers present before proceeding to “adjust” them in a manner that delivers a result far more palatable to the vegetarian cause.
OK folks, put your thinking caps on, and take a good look at the following:
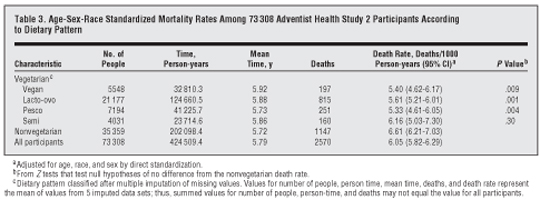
This is Table 3 from the AHS-2 paper. Without yet reading any of the fine print underneath the table, I want you to take a look at the figures in the column second from the right, the one titled “Death Rate, Deaths/1000 Person-years (95% CI)a“.
You’ll see that the researchers have cited mortality rates ranging from 5.33 to 6.16 deaths/1000 person years for the various vegetarian categories, while the lowly meat eaters return a rate of 6.61 deaths/1000 person years.
Here’s what you need to know about these death rate figures:
They’re complete bullshit.
And you’re now going to prove this to yourself, instead of taking my word for it. Grab your calculators, kids, it’s time for Debunking Epidemiological Hogwash 101.
Everybody got their calcs handy? Good. Let’s get to work.
The first thing we’re going to do is re-calculate the rate of deaths/1000 person years. This is pretty simple: Simply take the number in the “Deaths” column for each dietary category, divide it by the number in the “Time, Person-years” category, then multiply the resultant figure by 1000.
Doing so will give you the following deaths/1000 person years figures:
Non-vegetarian: 5.67
Vegan: 6.00
Pescovegetarian: 6.08
Lacto-ovo vegetarian: 6.53
Semi-vegetarian: 6.74
Now, take a good look at those figures and note who has the lowest death rate.
Yep, the non-vegetarians!
A similar result is returned when you calculate the number of deaths as a percentage of total number of participants in each dietary category (you can eliminate the difference in mean follow-up by multiplying each figure by the percentage 5.72 constitutes of the other longer mean follow-up periods).
No matter which way you work it, the raw data speak for themselves: The lowest death rate in the study is enjoyed by those who eat the most meat.
This, mind you, is despite the fact that the meat eaters clearly lived the unhealthiest lifestyles. They were far more likely to smoke cigarettes than the other categories, exercised less, got less sleep at night, and had higher BMIs. And yet they still exhibited the lowest mortality rate during the mean 5.7 year follow-up period.
That to me sounds like a pretty glowing endorsement of meat consumption, rather than a damning indictment!
The obvious question then, is how on Earth did the researchers arrive at their conclusion that vegetarians had lower mortality, and where on Earth did they derive the death/1000 year figures in Table 3?
Statistics, my friends, statistics.
Be Good to the Numbers and They’ll Be Good to You
Statistics are a lot like people: Rub them the right way, and they’ll often return the favour. Scratch their back, and they’ll scratch yours.
In fact, if you’re a real smooth operator, statistics are kind of like those girls who seem kinda shy at first, but with the right encouragement will proceed to do some shockingly raunchy stuff. Work them the right way, then once they’re sufficiently loosened up you can manipulate them into positions they would never normally go in their non-manipulated state. Darken the room, light some scented candles, play some Crazy P, start rubbing in the exotic oils, and those hot little numbers will promptly shed all their inhibitions, allowing them to freely perform the most unspeakable acts, in the process making all your wildest dreams an ecstatic reality.
Okay, okay, so epidemiologists don’t really use scented candles or essential oils or play Crazy P when they’re trying to bend the data in their preferred direction.
Instead, they use mathematical formulas.
Yep, who needs to waste time arranging velvety smooth sheets or selecting mood-enhancing tunes when you’ve got so many other statistical tools at your fingertips: Multivariate Analysis, Variance Components Analysis, Linear Mixed Models, Generalized Linear Models, Generalized linear mixed models, Loglinear Analysis, Kaplan-Meier Survival Analysis, Cox Regression Analysis, Time-Dependent Covariates, Regression Analysis, Multiple Regression Analysis, Curve Fitting…the list goes on and on.
And on.
Statisticians: They’d Like to Do it With the Entire Population, But Only Get a Small Sample
Let’s go back to Table 3 of the AHS-2 paper. We saw, before our very eyes, how running the numbers unmistakably returns figures showing lower mortality rates among non-vegetarians. Yet in the same table, the researchers present death rates showing the exact opposite.
So how did the researchers arrive at these numbers? Well, notice that little “a” next to “Death Rate, Deaths/1000 Person-years (95% CI)“? Look at the corresponding footnote underneath the table. It reads: “Adjusted for age, race, and sex by direct standardization.”
Welcome to the wonderful world of statistical manipulation, my friends. The only thing real and indisputable about this study is that the raw data show the lowest rates of mortality among non-vegetarians. Once the researchers take the data and start “adjusting” it, we move from the realm of concrete reality into the land of speculation, assumption, estimation and, all too often, outright bollocks.
So in Table 3, the researchers begin moving us into the latter realm by using a process known as direct standardization.
What, I hear you asking, is direct standardization?
If that sounds totally foreign to you, that’s the whole point. An essential part of pulling the wool over people’s eyes is using methods they don’t understand. This makes you seem real smart, a process encapsulated by the saying “If you can’t dazzle them with brilliance, baffle them with bullshit!”
Heck, I think I just summed up the entire field of statistics in one single sentence!
Can I go home now?
No? You want me to finish tearing this AHS-2 bollocks apart?
Bugger.
Alright, let’s continue…
To perform direct age standardization, one first has to select a reference population. The death rate in the population you are studying is then compared to the death rate recorded for the reference population. In the 7DA-2 paper, the researchers used the entire 7DA-2 study population itself as the reference.
Next, one computes the age-specific rates within the study group (in this case, each dietary category). Then, one multiplies these rates by the number of people in that age group in the reference population. These expected counts are summed and divided by the total population size of the reference population to yield the directly standardized rate.
Again, that probably sounds a bit foreign to many of you, but here’s the gist of what happened: The mean age of the 7DA-2 non-vegetarian sample was 55.9, in the other groups the mean age was 57.5-58.8. By using age standardization, the non-vegetarian group was penalized for having a mean age 1.6-2.3 years younger than that of the other groups. But would the results really have been much different if every group had, for example, a mean age of 57.58 (the average of the 5 groups)?
As for gender, the non-vegetarian group was middle of the field in terms on percentage of females, and second highest after the ‘pescovegetarians’ in percentage of blacks.
So again, what would the results have been if all groups had not only the same mean age but also the same number of female and black participants?
The only honest answer to that is that we don’t know. However, the researchers go ahead and claim otherwise, ignoring the raw deaths/1000 person-years data, running direct standardization and presenting the results as fact.
If the researchers had presented the raw data, then run the direct standardization calculations, then said something like the following, they would have been on much more honest ground:
“The raw data show that, despite their unhealthier lifestyles, non-vegetarians had the lowest death rates in the study. Adjustment of the data via direct standardization reversed these results, but we must emphasize that direct standardization is purely a paper exercise in speculation. Running a bunch of equations on our computers does not in any way change what actually happened in reality. And the reality is that non-vegetarians had the lowest mortality.
The only way to know if the results of the direct standardization analysis would hold up in real life is if we were able to re-conduct the study with five groups all sporting the same mean age/gender/race characteristics. Or even better, ditching this whole epidemiology wank and conducting a real study – i.e. a randomized controlled clinical trial that takes a large group of people and randomly assigns them to diets similar in every respect except that one contains meat and the other does not.”
But of course, the Loma Linda researchers didn’t say anything like this. Instead, having the direct standardized data they needed, they then proceeded to the next phase of their caper: Cox Regression Analysis.
Stop Fiddling with Cox, it’s Most Unbecoming
So now I hear you all asking: “Anthony, what the hell is Cox Regression Analysis?”
I must say, you’re a wonderful and very engaging audience, asking so many questions like this.
Cox Regression analysis was invented by a bloke called Sir David Cox, believe it or not. Sir Cox “observed that if the proportional hazards assumption holds (or, is assumed to hold) then it is possible to estimate the effect parameter(s) without any consideration of the hazard function.”
Again, that will sound like a load of gobbledegook to many of you, but all you really need to note here are the words “assumption”, “assumed” and “estimate”. Those words pretty much tell us everything we need to know. Or should already know. After all, it’s hardly a secret that humans are in no way omnipotent and cannot predict the future nor wave a wand and magically remove the influence of any and all confounders after the fact.
The best they can do is attempt to estimate the potential effect of confounding variables by using formulas based on assumptions.
In other words, they can guess. The fact that these guesses are based on sophisticated mathematical models still does not change one iota the fact that, ultimately, they are guesses.
Yep, a highly educated guess is still a guess, my friends.
And highly educated people, I might add, often screw up royally (a big hello at this point to every highly decorated researcher who has ever claimed saturated fat and cholesterol cause heart disease).
Anyways, so the Loma Linda researchers got their Cox on…oh wait, that didn’t sound right…um, they got to work with the Cox analyses in order to “adjust” for the effect not just of age/race/gender but also smoking, exercise, income, educational level, marital status, sleep and region.
The Cox analysis, remember, is an estimate of the impact of these various confounders, as is the Multivariate analysis that is also widely used in epidemiological studies.
Quick quiz:
Q: What are the formulas inherent in these analyses based on?
A: The results of other epidemiological studies.
Yep, epidemiology isn’t just your regular run-of-the-mill wank, folks – it’s a Ponzi-style wank!
And this elaborate multi-layered wankology, ladies and gentlemen, is how you take a set of raw actual figures and totally transform them into something they’re not. By the time they’re done, the Loma Linda researchers have managed to return 8-19% reductions from overall mortality in the vegetarian groups. Meanwhile, the hapless meat-eaters suddenly find themselves portrayed as having the highest death rate in the study from just about every listed cause!
Again, this wouldn’t be so outrageous if the researchers took pains to emphasize these reductions were purely speculative estimates arising from mathematical exercises. But they do the exact opposite, concluding:
“…vegetarian dietary patterns were associated with lower mortality. The evidence that vegetarian diets, or similar diets with reduced meat consumption, may be associated with a lower risk of death should be considered carefully by individuals as they make dietary choices and by those offering dietary guidance.”
What the Loma Linda researchers want us to believe is that, despite having the lowest mortality rate in the study, non-vegetarians actually had the highest death rate in the study!
Got that?
And they further believe that people issuing dietary advice to the public should seriously consider basing their recommendations on this fantasy-based nonsense!
Holy cow.
Why Vegetarians Don’t Like Clinical Trials
The Loma Linda team have been publishing papers for almost forty years now, many claiming reductions in mortality, heart disease and cancer to be associated with vegetarianism.
Like most of their epidemiological brethren, these researchers seem utterly unwilling to acknowledge the speculative nature of their work, and totally oblivious to the fact that statistical associations are just that: Statistical associations.
I’ve already said this 1,000 times, and I’ll no doubt say it another 1,000 times, but the first rule of good science is…that…
ASSOCIATION DOES NOT EQUAL CAUSATION!
Breathe Anthony, breathe LOL
So here’s my advice to the folks from Loma Linda University and EPIC-Oxford, along with all those who incessantly cite epidemiological associations as if they constitute solid evidence of the superiority of vegetarian diets:
Quit the statistical chicanery, and take the large amount of tax money you waste on this epidemic of epidemi-hogwash and instead use it to conduct some real studies. That is, randomized controlled clinical trials in which large groups of participants are randomly assigned to one of two diets similar in every respect except that one contains meat and the other doesn’t. Go ahead and throw in a fish-eating diet as well if it makes you feel better, but for crying out loud just don’t call it “pescovegetarian”.
You vegetarian proponents have actually had decades to do this, but with a few small exceptions have shunned the opportunity. Instead, you’re happy to keep supporting your dogma by citing distorted data from confounder-prone epidemiological studies involving health-conscious vegetarians versus health-indifferent omnivores.
Why is that I wonder?
Let’s take a look at those few small exceptions I just mentioned to find out.
Vegetarian Diets on Trial
The EPIC study shows that, despite their healthier lifestyle habits, vegetarians experience a slightly higher mortality rate than their omnivorous peers. And the raw unadulterated data from AHS-2 suggests the exact same thing. Far from providing support for the highly-hyped superiority of vegetarian diets, these results suggest that vegetarian diets are so nutritionally inferior they completely negate the benefits of exercise, non-smoking, good sleep habits and lower BMI and alcohol consumption.
And, lo and behold, the clinical research performed to date supports this very contention.
Despite all the lavish claims made for vegetarianism, there is amazingly little long-term clinical research directly comparing their effects on cardiovascular disease, cancer and overall mortality with omnivorous diets. The randomized clinical trial evidence in this genre pretty much begins and ends with two small studies, one published by Dr Dean Ornish and the other by a group of Oregon researchers.
Ornish’s trial, the Lifestyle Heart Trial, was published back in 1990. This is the same clinical trial that provided the springboard for the well-known low-fat and vegetarian author to launch a lucrative career claiming he could reverse heart disease. This claim is made despite the fact that Ornish’s intervention has completely failed under randomized controlled conditions to save even a single life.
Ornish’s “Lifestyle” program actually involves several interventions aside from the omission of meat. Participants are counselled to exercise, engage in stress reduction activities, and to cut all the refined and heavily processed junk from their diets. All these factors on their own could have a significant and favourable impact on CHD risk, but despite these confounding factors Ornish routinely cites his intervention as proof of the efficacy of meat-free and low-fat diets.
But just how effective is his program, anyway?
After one year of follow-up in the Lifestyle trial the researchers reported 82% of those in the experimental group experienced regression of arterial plaque, compared to only 42% of those in the control group, as determined by angiography. The experimental group subjects also experienced significantly less chest pain[12]. But these factors could easily be due to exercise and stress reduction.
In 1998, the Journal of the American Medical Association published the five-year follow-up data for the Lifestyle Heart Trial. While the experimental group experienced a significantly reduced overall incidence of cardiac events (a composite classification that included angioplasty, bypass surgery, heart attack, and hospitalization for any cardiac cause), the treatment group actually experienced one more death than the control group (two people in the intervention group died compared to one person in the control group)[13].
Ornish claims that one of the treatment group deaths was in a participant who had stopped following the intervention. Another intervention subject allegedly got a little too enthusiastic whilst exercising, exceeding his prescribed target heart rate with fatal consequences. So it would seem luck just wasn’t on the intervention group’s side during the Lifestyle Heart Trial.
However, a similar scenario unfolded during the trial by Oregon researchers. This trial involved what the authors referred to as the “PrimeTime” program, which incorporated Ornish’s vegetarian “Reversal” diet, exercise, smoking cessation, and daily stress reduction activities (meditation, relaxation, deep breathing, visualization). Twenty eight women with pre-existing CHD were successfully recruited for the study, 16 of whom were randomized to the treatment group. The remaining twelve women in the control group continued to receive usual care from their own doctors.
A 2000 report hails the intervention as a great success, reporting a reduction in hypertensive medication dosage among the PrimeTime participants. The researchers also noted that chest pain frequency decreased in this group throughout the 2-year study, but a look at the data shows chest pain severity increased in both groups, though this did not reach statistical significance in either group. Other peculiarities include not only an increase in severity but also the duration of chest pain in the PrimeTime group at 4 months, despite frequency of chest pain reportedly having been reduced markedly at this point. These discordant results are probably explained by the fact that chest pain frequency, severity and duration were attained via questionnaires administered to the patients, and therefore highly susceptible to the vagaries of subjective recall.
The incidence of actual heart attack and stroke were not reported in the study, but the researchers did report on the most important and objective outcome of all:
Death.
One patient in the intervention group died of a heart attack. Another two PrimeTime subjects had to withdraw from the study due to “discomfort with the program”, but the researchers do not elaborate; whether this referred to adverse health effects or inconvenience arising from the intervention is unknown.
Meanwhile, all the control subjects survived and completed the two-year follow-up[14].
And that, ladies and gentlemen, pretty much constitutes the entire body of randomized controlled clinical evidence comparing cardiovascular and overall mortality outcomes among participants following vegetarian and omnivorous diets. In both trials, the treatment groups had the advantage of being compared to people who were doing little to no exercise and not receiving any specialized dietary advice, not engaging in any structured stress relief strategy, nor participating in regular and dedicated counselling. Despite the highly touted improvements in so-called “risk factors”, both intervention groups experienced higher mortality rates.
Actually, the story doesn’t quite end with these two small trials. There is one more study comparing participants on Ornish’s program, but it wasn’t a randomized trial. The Multicenter Lifestyle Demonstration Project sought to apply the intervention in Ornish’s original trial to a larger group of patients recruited from clinics across the U.S. Practitioners from eight medical centres around the country were trained in all aspects of the Lifestyle program, which they proceeded to administer to patients with coronary artery disease. As noted, the study was not conducted in the manner of a randomized, controlled trial; instead, outcomes in the 194 patients who completed the intervention were compared with 139 patients who did not take part in the Lifestyle program but had recently undergone revascularization procedures.
So did the Lifestyle program finally deliver its claimed lifesaving, heart disease-reversing benefits?
Nope.
After three years, there were no significant differences in cardiac event rates or mortality between patients in the intervention and control groups. The number of cardiac events per patient year of follow-up when comparing the experimental group with the control group was as follows: 0.012 versus 0.012 for myocardial infarction, 0.014 versus 0.006 for stroke, 0.006 versus 0.012 for non-cardiac deaths, and 0.014 versus 0.012 for cardiac deaths (none of the differences were statistically significant)[15].
Again, this is despite the fact that the Lifestyle participants received dedicated counselling, lost weight and improved their exercise tolerance. No corresponding data were given for the control group, but given the absence of the intense counselling afforded to the intervention group, it is unlikely that the former would have experienced such changes – a contention supported by the original Lifestyle trial.
In his 1998 paper reporting on the MCLP results, Ornish writes as if these uninspiring results were a great success. His reasoning is that his program is cheaper than revascularization, yet produced similar coronary event and mortality rates. Because 150 of his 194 patients avoided revascularization (44 still had to be wheeled into the operating theatre during the 3-year study), Ornish’s selling point in the paper is that his program is a cheaper alternative to revascularization.
That all sounds great, but if you’ve read The Great Cholesterol Con you’ll know when revascularization is put to the test in RCTs, it has repeatedly failed to show any mortality advantage and some studies have actually shown a slight disadvantage, when compared to patients receiving standard non-invasive medical care. So, in effect, Ornish’s 1998 paper is boasting that his program is no more effective but at least cheaper than another largely ineffective option.
Remember, Ornish’s program included exercise, and we know that an intelligently prescribed exercise program can do wonders for cardiovascular health, even in those that have already suffered a heart attack. In the March 2004 issue of Circulation, German researchers reported on a study in which 101 male patients with stable coronary artery disease were randomized to either undergo stent angioplasty or to participate in an exercise-training program. For the first two weeks, those in the exercise group trained in the hospital 6 times a day, 10 minutes at a time, on a stationary bicycle at 70% of their symptom-limited heart rate (the symptom-limited heart is the heart rate at which evidence of ischemia becomes apparent during an exercise test; needless to say, this should be ascertained during a professionally supervised session).
After this initial two-week period, the exercising patients took their stationary bikes home with them. They were asked to cycle at the prescribed heart rate for twenty minutes per day, and to participate in one 60-minute group aerobic exercise session each week.
The aim of the study was to see which strategy produced the most favourable effect on clinical outcomes – including heart attack, stroke, hospitalization for worsening angina, surgery or further angioplasty – during a twelve-month follow-up period. Thankfully, none of the patients died, but when the final data was tallied, it was observed that 21 of the 50 patients who underwent PCI had a subsequent coronary event, as compared to only 6 of the 51 exercising patients – a highly significant difference.
The exercisers also experienced far greater improvements in maximal exercise tolerance, and were 32% less likely to experience progression of atherosclerosis. Furthermore, the superior results seen in the exercise group were achieved at half the cost necessitated by the PCI procedure[16].
Vegetarianism: The ‘Healthy’ Way to Die Sooner?
What is apparent from the aforementioned Lifestyle and PrimeTime studies is that, despite their inclusion of proven treatments such as exercise and weight loss and the strong link between stress and coronary disease, Ornish’s vegetarian diet still failed to reduce the incidence of heart attack, stroke or coronary mortality. This would indicate that a meatless diet actually negates the effect of the other positive aspects of his intervention.
To put it another way, vegetarian diets have a number of known nutritional pitfalls and, similar to the epidemiological research, the Ornish and PrimeTime studies indicate these pitfalls are so detrimental they cancel out the benefits that would normally be expected from exercise, weight loss, elimination of junk food, and stress reduction.
Stay tuned for Part 2, where we’ll discuss these pitfalls in all their gory detail.
Disclosure Statement: The author of this article has absolutely no relationship, financial or otherwise, with the meat, dairy, or egg industries. The author, according to the bizarre Loma Linda University system of dietary classification, is a “carno-pesco-lacto-ovo-vegetarian”, which means he enjoys a bloody good steak on a very regular basis.
References
- Gardener H, et al. Coffee and Tea Consumption Are Inversely Associated with Mortality in a Multiethnic Urban Population. Journal of Nutrition, 2013 jn.112.173807; first published online Jun 19, 2013.
- Phillips RL. Role of lifestyle and dietary habits in risk of cancer among Seventh-Day Adventists. Cancer Research, Nov, 1975; 35: 3513-3522.
- Fraser GE. Associations between diet and cancer, ischemic heart disease, and all-cause mortality in non-Hispanic white California Seventh-day Adventists. American Journal of Clinical Nutrition, Sep, 1999; 70 (3): 532S-538S.
- Berkel J, de Waard F. Mortality pattern and life expectancy of Seventh-Day Adventists in the Netherlands. International Journal of Epidemiology, Dec, 1983; 12 (4): 455-459.
- Fønnebø V. The healthy Seventh-Day Adventist lifestyle: what is the Norwegian experience? American Journal of Clinical Nutrition, May, 1994; 59 (5 Suppl): 1124S-1129S.
- Zollinger TW, et al. Breast cancer survival rates among Seventh-day Adventists and non-Seventh-day Adventists. American Journal of Epidemiology, Apr, 1984; 119 (4): 503-509.
- Fraser GE. Determinants of ischemic heart disease in Seventh-day Adventists: a review. American Journal of Clinical Nutrition, Sep, 1988; 48 (3 Suppl): 833-836.
- Mills PK, et al. Dietary habits and breast cancer incidence among Seventh-day Adventists. Cancer, Aug 1, 1989; 64 (3): 582-590.
- Mills PK, et al. Animal product consumption and subsequent fatal breast cancer risk among Seventh-day Adventists. American Journal of Epidemiology, 1988 Mar; 127 (3): 440-453.
- Mills PK, et al. Cancer incidence among California Seventh-day Adventists, 1976-1982. American Journal of Clinical Nutrition, 1994: 59 (suppl): 1136S-1142S.
- Orlich MJ, et al. Vegetarian Dietary Patterns and Mortality in Adventist Health Study 2. JAMA Internal Medicine. Published online Jun 3, 2013. doi:10.1001/jamainternmed.2013.6473
- Ornish D, et al. Can lifestyle changes reverse coronary heart disease? The Lifestyle Heart Trial. Lancet, Jul 21, 1990; 336 (8708): 129-133.
- Ornish D, et al. Intensive Lifestyle Changes For Reversal of Coronary Heart Disease. Journal of the American Medical Association, Dec 16, 1998; 280 (23): 2001-2007.
- Toobert DJ, et al. Physiologic and related behavioral outcomes from the women’s lifestyle heart trial. Annals of of Behavioral Medicine, 2000; 22 (1): 1-9.
- Ornish D, et al. Avoiding Revascularization with Lifestyle Changes: The Multicenter Lifestyle Demonstration Project. American Journal of Cardiology, Nov 26, 1998; 82 (10B): 72T-76T.
- Hambrecht R, et al. Percutaneous Coronary Angioplasty Compared With Exercise Training in Patients With Stable Coronary Artery Disease: A Randomized Trial. Circulation, Mar, 2004; 109: 1371-1378.
—
Anthony Colpo is an independent researcher, physical conditioning specialist, and author of The Fat Loss Bible and The Great Cholesterol Con. For more information, visit TheFatLossBible.net or TheGreatCholesterolCon.com
Copyright © Anthony Colpo.
Disclaimer: All content on this web site is provided for information and education purposes only. Individuals wishing to make changes to their dietary, lifestyle, exercise or medication regimens should do so in conjunction with a competent, knowledgeable and empathetic medical professional. Anyone who chooses to apply the information on this web site does so of their own volition and their own risk. The owner and contributors to this site accept no responsibility or liability whatsoever for any harm, real or imagined, from the use or dissemination of information contained on this site. If these conditions are not agreeable to the reader, he/she is advised to leave this site immediately.
Lies, Damned Lies, and Vegetarianism: Part 1. « AnthonyColpo.